The Miscarriage Dialogues: Fertility Expert Alex Johnston on Early Fertility Awareness and the Future of IVF in the U.S.
Fertility expert Alex Johnston warns of IVF access threats, the urgent need for early fertility awareness and shares how to protect your choices before it’s too late.
At Miscarriage Movement, we believe that knowledge is power—especially when it comes to reproductive health. Yet, for so many women, the first time they truly confront the realities of fertility is after experiencing miscarriage or infertility firsthand. By then, vital information about their reproductive health—like egg quality, ovarian reserve or underlying conditions like PCOS, endometriosis or autoimmune conditions—has been withheld, dismissed or simply never offered.
This is the exact crisis that fertility expert, advocate and author Alex Johnston is working to change.
Johnston has been sounding the alarm about the lack of fertility education for years, advocating for early fertility awareness so women have the information they need long before they face challenges trying to conceive. After her own heart-wrenching journey through pregnancy loss, infertility, surrogacy and ultimately giving birth to a baby boy, she knows firsthand the life-altering impact of delayed fertility education—and she’s determined to ensure fewer women have to learn the hard way.
But right now, fertility care is facing a new, urgent threat.
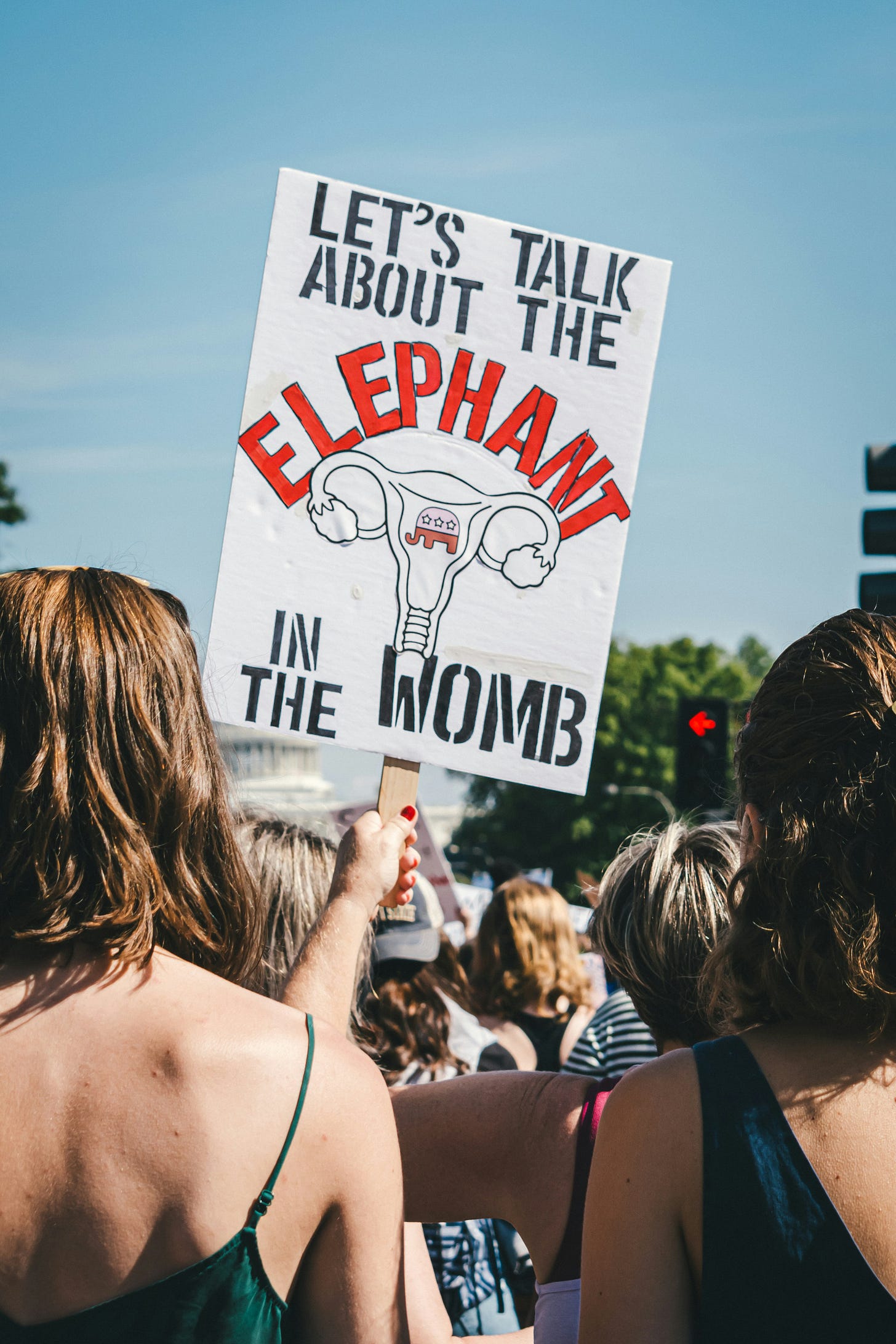
With the current Trump administration and new healthcare leadership that’s taken power, access to IVF and other fertility treatments may soon be in serious jeopardy. Restrictions on reproductive healthcare—including contraception, fertility treatments and surrogacy—could make family-building even harder for those who need medical assistance to conceive.
In this critical moment for reproductive rights, Johnston joins us for an unfiltered conversation about:
The biggest fertility misconceptions that lead women to delay crucial testing
Why early fertility awareness is essential—even if you’re not ready for kids yet
How IVF access could be threatened under new leadership, and what that means for hopeful parents
What women can do to advocate for their reproductive rights in the face of uncertainty
This is a conversation every woman needs to hear—whether you’re trying to conceive now, planning for the future or simply want to protect your reproductive choices.
Read on for our full discussion with Johnston, and let’s keep pushing for better fertility education, support and access—before it’s too late.
What are some of the biggest misconceptions people have about fertility health and how can more awareness help women navigating miscarriage or recurrent loss?
The biggest issue is the lack of fertility education for young women, leaving them unaware of what questions to ask and when to seek answers.
In my early teens, I had ample access to information about menstruation and birth control—issues that were very relevant to me at that age—but there was very little focus on fertility and risk of infertility.
Once I was thinking about having a baby, the main misconception I encountered was the sense that age 35 was a fertility-dividing line and that your fertility really only started to decline then. When I finally did see a fertility specialist, two years after starting to try, was the first time I learned the kind of relevant information I needed: that, on average, a woman’s fertility starts to decline by the end of her twenties, and by the age of 32 (the age when I started trying to get pregnant), 15 percent of women would struggle with infertility, making it hard or impossible for them to get pregnant. I also needed to know that getting my own fertility information through some basic and inexpensive medical tests is really easy. That information would have helped me make better-informed choices about when to start trying and to seek out help much earlier than I did.
Every woman’s fertility is unique to her so getting information about your own body through fertility testing—i.e. the quality of your eggs, the number of eggs you have left in your ovaries and the thickness of your uterine lining to allow an embryo to attach and grow—are the kinds of things that help women understand what they may be up against.
I discovered I was unable to carry, so I worked with surrogates to have my first two children. Having the relevant information much earlier would have probably saved me a lot of heartache. Through a miracle, I discovered I was pregnant shortly after having my two girls, and I gave birth to my son naturally.
With the current administration and shifts in healthcare leadership, what are the most immediate threats to IVF access and fertility treatments?
Early education needs to start for girls in their early teens so we can normalize this conversation. That means bringing this into schools, and in the current political climate, it feels unlikely that many states would do that and more likely that many families would find that to be an overreach for what schools should be teaching girls.
Most people don’t think they will have a problem. When we were mostly having babies in our twenties, infertility and miscarriage were less of an issue. But the majority of babies in the U.S. now are born to women in their thirties, so infertility and pregnancy challenges like miscarriage and pregnancy loss are now big issues. And girls and young women need to learn more about them. Any state that is serious about helping children understand their bodies, their health, and the significant issue that infertility represents for young people today should start the education process early and normalize this issue as part of a health curriculum.
Once women are out of school, the main place they will find information is in a medical setting like their family doctor’s office. So physicians need to be armed with the right information and comfortable sharing this with women early enough for it to be useful. Waiting until a woman first raises the desire to have a baby is too late. This information needs to be shared early, routinely in visits to physicians, and a fertility work up should be offered as a standard part of a woman’s annual check-up – similar to how we have normalized a pap test – so that she can start tracking her fertility by her late twenties. These are not expensive steps, so cost is not the issue.
Awareness and understanding of the significance of this major health issue, the crushing impact it has on women and men, and the simple steps we can take to help solve it is the conversation we want to be having.
For women currently undergoing fertility treatments, what should they be watching for in terms of potential policy changes that could affect their care?
Coverage is the biggest policy change to look for. Making sure as you move down this road that you understand what is covered in health plans and what is not. It can be a very expensive undertaking.
If IVF were to become more restricted or even banned in certain states, what alternatives or proactive steps should women and couples consider now?
If restricting access to IVF becomes a reality in the US, then looking to other countries, like Canada, will be necessary. I am a Canadian living in Toronto. I worked with surrogates in Canada and the US. We did most of our treatment in Canada, and one of my children was born in the US. Fertility help in Canada and other countries is and will remain a viable option for Americans to seek help if the situation in the US changes.
I have always been touched by how active and helpful the infertility community is. I still get contacted throughout the year by people looking for guidance around surrogacy. I recently connected the daughter of one of my US surrogates to a couple, and she acted as a surrogate for them to carry their child. The infertility community is broad, international, strong, supportive and committed to helping others. Wherever the US goes on this issue, there are lots of countries, like Canada, that are not moving in that same direction.
What can those impacted by infertility do right now to advocate for their rights, both legally and politically?
Infertility doesn’t have neat categories. It cuts across communities, political parties and religions. It doesn’t choose you by race or income level. It doesn’t distinguish between good parents and bad parents, good people and bad people. Everyone knows someone who has experienced it – a friend, child, sibling, grandchild, co-worker. It is a tough, tough road to travel. Those who have been down that road have the battle scars to show for it, and the people who care about them probably do too. It is hard to watch someone you care about suffer.
Anyone who understands this experience should make a point of speaking about it publicly when they can. Know the facts and share them within your community. If someone perpetuates ill-informed stereotypes about why people face infertility—for example, that women who face it waited too long to have a baby—set them straight. This is now a major health issue because the majority of women and men are choosing to have children in their thirties. There are biological realities that go along with that demographic shift such that more and more women and men will face this. Advocate within your company for insurance coverage for treatment help and medication.
First and foremost advocate for yourself. Get your own health information about your own fertility so you know what you may be up against. Ask questions and get the answers you need so you can make informed choices.
And keep normalizing this conversation by talking about it as the important health issue it is.
You’ve been open about your own experiences with infertility, pregnancy loss and surrogacy. How did those experiences shape your advocacy and the work you do today?
I have always been open, partly because I was doing surrogacy twenty years ago well before it was part of the infertility mainstream. I was the only person most people in my personal and professional communities knew who was pursuing surrogacy, so I was on the receiving end of many questions and spoke openly about the challenges and the experience.
There was clearly a lot of misinformation, not just about surrogacy, but infertility in general. People would ask me if my husband and the surrogate had to have sex to create the baby—or if I was afraid I wouldn’t be able to love my child because I wasn’t carrying the child. They would offer advice on my exercise routine and work stress and a range of things I could do to help myself get pregnant as if somehow I was doing something wrong that I could correct and things would get better.
Once I began working with a fertility specialist and grasped the staggering prevalence of infertility among women in their thirties, it became clear just how much greater awareness was needed. At the time, I held a senior role in government, giving me the platform to influence policy. Recognizing the urgency of this issue, I became a vocal advocate—not just for myself, but for broader systemic change. Alongside other dedicated voices, I helped lay the groundwork for significant policy reforms around infertility in Ontario.
When I was on the other side of infertility with my own family, it became clear to me that young women were still getting terrible advice and guidance—or none at all—on infertility, so I decided to write a book. I would’ve loved to write a book full of facts and data about infertility, but it turns out, I am one of only a handful of people who really love that kind of thing. So I wrote my own story, based on the profoundly life-shaping, often painful, sometimes heartbreaking and ultimately beautiful journey that was my family-building experience.
By the time I wrote my book, my own family-building journey was behind me, but I couldn’t stand by and watch another generation of young women step into this process as unprepared as I once was—without the information or support they deserve. Infertility is, in many ways, a quiet epidemic, affecting more people than we acknowledge. We have to do better. Every young person who hopes to become a parent one day should have access to relevant, timely fertility information—before it’s too late to act on it.
What are some of the biggest emotional hurdles women face when going through infertility or pregnancy loss, and how can we create more supportive spaces for these conversations?
I think it’s very personal for each person and experiences differ. I had a hugely supportive family, friend network and work community. Yet, I still found it totally isolating. Our experience was compounded by the loss of our first child who was stillborn. My grief separated me from most of my peers. My husband and I really had to turn towards each other to survive some very painful years. I think the inability to have a child when you want to, pregnancy loss or stillbirth is a uniquely painful experience. I had never wanted anything as much as I wanted to become a parent once I started down this road. Watching my friends do this thing so effortlessly, but with a completely different experience and outcome than me, felt random and unfair. I didn’t wish it on anyone else but I had to distance myself from many people for self-preservation.
Real understanding and awareness really helps. I have always said that the audience for my book isn’t women who have gone through infertility. They lived it firsthand so they know what the experience is like. It is for people who haven’t gone through this but who do want to understand. I wish my parents, my friends, my colleagues, and others had a book like this when I was going through it. Caring about someone experiencing loss isn’t enough. Caring about them in the way they need to be cared for requires understanding and knowledge and awareness of their experience can help with that.
Despite growing awareness, there’s still so much stigma around infertility and pregnancy loss. What do you wish more women—and healthcare providers—understood about these struggles?
Much of this is preventable. Women need accurate, timely fertility information—not when they’re already struggling, but early enough to make informed choices. Fertility testing should be a routine part of annual medical check-ups, just like any other key health screening. Physicians shouldn’t wait for patients to bring it up—these conversations should be proactive, ensuring women have the knowledge they need to navigate their reproductive health with confidence.
Make the following facts available widely – in schools, universities and colleges; in workplaces; in doctors' offices; at health conferences; in discussions around company health plans. Share them like your life depended on it:
The majority of babies today are born to women in their thirties.
A woman’s fertility starts to decline by her late twenties.
By age 32, fifteen percent of women will face infertility.
Fertility testing is easy to do and available through your family doctor.
The best thing we can do for women is help them avoid challenges in having children. The next best thing we can do is support them when they do by making sure awareness is widespread so their experience is understood and treatment is available and affordable to help them build their family.
The financial burden of fertility treatment is often overwhelming. What advice do you have for those navigating the high costs of IVF, egg freezing or other treatments?
Get the facts about your own situation. Know what you are up against. Don’t keep trying the same thing over and over hoping the outcome will be different. Understand your options and make informed decisions once you know what is covered and what is not so you get on a path that is financially manageable for you as soon as possible. Don’t delay getting help. The longer you struggle the harder it is.
How do we push for better insurance coverage and more equitable access to fertility care in the U.S.?
This is a young person’s health issue and, based on the demographic shift in pregnancy and rates of infertility for women by their thirties, a lot of young people will face it. Every young person in the U.S. should be advocating for better insurance coverage for their generation. Health spending is disproportionately skewed to the last years of people’s lives. The needs of young people need to be better reflected in our health spending. This issue is an important one that cuts across communities, political parties, state lines, religions, races and finances. Companies have made a lot of progress here in the last 5-10 years. Fertility benefits are in more plans and for higher amounts than ever before.
I would say to any insurance executive or politician in the U.S. today that if children are as important as we say they are then we need to back that up with our actions and not just our words. Better support for people needing help building their families is a great place to start.
As a culture, how do we need to shift our thinking about fertility struggles and family-building to make these challenges less isolating and more supported?
That is a tough one. I did have access to a mental health professional who helped me. With limited access to mental health support in many places, people need to look for other ways of supporting their mental health. They are not alone. The stories that people share, through books, movies, and, in many cases, online forums can be helpful. My mantra was to try to manage the things that I could manage—eat, sleep and exercise. I found my people to go through this with and hung on for dear life through a very bumpy journey. Thankfully, they hung on to me just as hard. I made a decision, especially after our stillbirth, to go back to work because I needed a focus outside my home and my grief. I let my boss know what I was managing and found support at work but I had a good sense that my workplace would be supportive.
Understanding really is the foundation of support. Without that, it is hard to offer the person the type of support that is meaningful and useful to them. For anyone going through this, I would say find people who can add value to your world—that may be friendship, food, humor, financial support, or a sounding board—and build the community of the willing who can help you through this. For anyone wanting to support someone going through this, I would say to love the person the way they need to be loved, which may be different from how you want to love them. Find ways to add value to become part of their community of the willing.
These conversations matter, and so does your voice.
If you have a story to share, an idea to pitch or just want to reach out, we’d love to hear from you. Email us at jenn@milaandjomedia.com or send us a DM at @miscarriagemovement.
Talking about miscarriage shouldn’t feel like a secret. Let’s keep pushing for change—together.